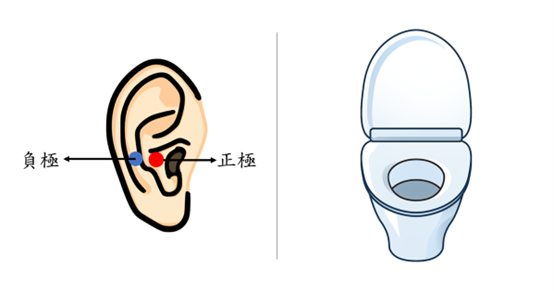
在歐美,泌尿科疾病之盛行率達11.8%-35.6%,其中又以女性較多,由於長期症狀影響生活品質和睡眠,並增加身心疾患風險,其中有部分對藥物並無反應,屬於難治型患者,因此需要開發其他替代療法來改善症狀。taVNS通過耳廓電刺激迷走神經分支,非侵入式且便攜,對癲癇、憂鬱、耳鳴、頭痛有效。
研究顯示taVNS調控大腦內感受迴路,影響視丘、島葉、杏仁核、前扣帶皮層、前額葉等腦區,提高副交感神經活性,與自主排尿控制迴路高度重疊,因此可能減緩泌尿系統疾病之症狀。
本研究案為跨領域合作,整合台南醫院泌尿科、成大醫院泌尿科、神經內科之生醫專業以及本實驗室之資訊工程專業,探討taVNS對泌尿疾病之療效,並探索taVNS的治療機轉。本實驗預計招募25名泌尿疾病患者,受試者將進行每週兩次taVNS,為期四週的治療。
在治療前、治療中、治療後等三個階段,我們會蒐集患者之泌尿功能、生化檢測和腦部活動,以針對以下三個研究主題來個別解析:
taVNS治療後泌尿功能改變
taVNS治療後神經免疫和生化指標變化
taVNS治療後大腦排尿控制中樞神經活動變化
In Europe and the United States, the prevalence of urological disorders ranges from 11.8% to 35.6%, with a higher incidence among women. These conditions can severely impact quality of life and sleep, increasing the risk of both physical and mental health issues. Some patients, particularly those who do not respond to medications, represent a challenging group in need of alternative therapies.
Transcutaneous auricular vagus nerve stimulation (taVNS) offers a non-invasive and portable treatment option that has shown effectiveness in conditions such as epilepsy, depression, tinnitus, and headaches. Research indicates that taVNS modulates sensory circuits in the brain, affecting areas like the thalamus, insula, amygdala, anterior cingulate cortex, and prefrontal cortex. This modulation enhances parasympathetic activity and aligns with autonomic bladder control pathways, potentially alleviating symptoms of urological disorders.
This study is a multidisciplinary collaboration involving the urology departments of Tainan Hospital and NCKU Hospital, the neurology department of NCKU Hospital, and our lab. The goal is to explore the efficacy of taVNS for treating urological disorders and to investigate its underlying mechanisms.
We plan to recruit 25 patients with urological conditions, who will receive taVNS twice a week for four weeks. Data will be collected at three stages: before, during, and after treatment. We will gather data on urological function, biochemical markers, and brain activity. The study will focus on the following research areas:
Changes in urological function following taVNS treatment.
Variations in neuroimmune and biochemical markers after taVNS treatment.
Alterations in brain activity related to urinary control after taVNS treatment.